When working in the healthcare sector, dealing with sensitive patient information is par for the course. But as a healthcare product manager or app developer, do you know the ins and outs of managing this data?
This is why the HIPAA release form was instated. It's a pivotal tool for ensuring patient and customer data safety.
This guide is tailored specifically for developers and product managers looking to demystify HIPAA regulations, understand HIPAA release forms, and seamlessly integrate them into healthcare applications or systems.
What's a HIPAA release form?
A HIPAA release form is a document that a patient fills out to grant permission for healthcare providers to disclose specific types of personal health information (PHI).
The Health Insurance Portability and Accountability Act (HIPAA) is a US federal law enacted in 1996. It protects patients' medical records and other health information provided to healthcare providers, health plans, and health insurers.
This information can be released to another healthcare provider, a family member, or any third party specified by the patient.
Why is a HIPAA authorization form important?
Navigating the intricate healthcare data ecosystem demands more than coding knowledge. It requires a keen understanding of the regulatory landscape.
A HIPAA authorization form is the legal and ethical backbone that supports transparent, secure data exchanges between healthcare entities, patients, and third-party services.
Let's explore why this document is indispensable for respecting patient choices and streamlining interoperable healthcare solutions.
Giving informed consent for the disclosure of health information
In the interconnected world of healthcare, exchanging patient data between various entities is commonplace. While this interconnectedness offers incredible benefits for the efficiency and effectiveness of patient care, it also raises essential questions about privacy and agency.
That's where informed consent, facilitated through a HIPAA authorization form, becomes vital.
For patients, informed consent serves as an empowerment tool. It gives them control over who sees their medical records, for what purpose, and under what conditions. This fosters a sense of ownership and agency, which is crucial for building their trust in healthcare systems and providers.
For healthcare providers, obtaining consent from patients isn't just a procedural necessity – it's the cornerstone of ethical practice. It enables transparent communication, helps set accurate patient expectations, and underscores the provider's commitment to respecting patient autonomy.
In essence, informed patient consent bridges the gap between technological capability and ethical responsibility. It's the safeguard that ensures the power to share data comes with the responsibility of respecting individual choices.
Providing protected health data
With the increasing amount of healthcare-related data breaches, maintaining the integrity of patient information is more crucial than ever. A properly executed HIPAA release form ensures that information is only shared when explicitly authorized, enhancing trust and data security.
A HIPAA release form is a formalized framework specifying who's authorized to access, use, or disclose PHI. It streamlines the consent process and ensures that only individuals or entities expressly approved by the patient can interact with their data.
This reduces the potential for unauthorized access and creates an audit trail to maintain data integrity.
Interoperability
In healthcare, sharing information quickly and securely can be a life-or-death situation. HIPAA release forms facilitate this by setting the legal framework for data sharing between various healthcare providers and third parties.
These forms set the legal boundaries for how patient data may be shared among healthcare entities and third-party service providers. Without HIPAA authorization forms, seamless data exchange would be a logistical and legal nightmare. This can hinder care coordination and slow down medical processes.
Information silos are a barrier to efficient healthcare delivery. HIPAA release forms allow for authorized, purpose-driven data sharing, reducing the instances where critical patient information is locked away in one part of the healthcare system and inaccessible to another where it might be urgently needed.
Interoperable systems, underpinned by patient authorizations, also help maintain accurate and up-to-date patient records.
When information can flow freely and securely, healthcare providers are less likely to rely on outdated or incorrect data and minimize the risk of medical errors.

Who needs to use a HIPAA release form?
The HIPAA is a US federal law, so its primary jurisdiction is within the United States but also extends to the following US territories:
- Puerto Rico
- Guam
- US Virgin Islands
- American Samoa
- Northern Mariana Islands
The Act applies to healthcare providers, health plans, and healthcare clearinghouses (known as "covered entities") and their business associates. This includes doctors, laboratory technicians, hospitals, insurance companies, wellness apps, and billing services.
In this sense, a HIPAA release form isn't only for doctors or hospital staff. These forms are crucial for anyone dealing with healthcare data, including health and wellness app developers.
So, who really needs this form in their day-to-day work? Let's find out.
- Healthcare providers and entities
- Health software and app developers
- Third-party vendors
- Business associates abroad
- Treatment of US citizens abroad
- Cloud storage and data centers
- Telemedicine services
Healthcare providers and entities
Any healthcare entity that collects, stores, or processes PHI falls under the umbrella term "healthcare providers." Healthcare providers like hospitals, clinics, and doctors must use HIPAA release forms to gain consent and protect patient data.
Health software and app developers
Developers creating applications that interact with healthcare data must also know when to implement HIPAA release forms. This is especially important for telemedicine apps, patient portals, and Electronic Health Record (EHR) software.
Third-party vendors
Companies that provide services to healthcare entities, like cloud storage providers or billing companies, may also need to use HIPAA release forms if they can access or manage PHI.
Business associates abroad
If a US-based covered entity works with a business associate in another country, that associate must comply with HIPAA regulations concerning any PHI they handle or process.
Treatment of US citizens abroad
If a US citizen seeks medical treatment abroad and the foreign healthcare provider transfers health records to a US-based entity, it may necessitate HIPAA compliance. Note that the foreign provider itself isn't directly bound by the HIPAA.
Cloud storage and data centers
US-based covered entities using cloud storage services or data centers located outside the United States to store PHI may need HIPAA release forms. The international data storage service provider is considered a business associate and needs to comply with HIPAA regulations.
Telemedicine services
Some telehealth services may involve cross-border data transfer. In such cases, any US-based entity must ensure their foreign business associates comply with HIPAA.
Telemedicine involves providing healthcare services through digital platforms, often enabling patients and healthcare providers to interact without being in the same physical location. For instance, a US-based doctor may consult a patient traveling internationally.
This technology has been a game-changer, especially in improving access to medical care for people in remote locations or those who can't easily visit a healthcare facility.
What happens when you don’t have a signed HIPAA release form?
There may be some severe repercussions if you fail to provide signed HIPAA release forms to prove patient data sharing consent. From legal problems to roadblocks in patient care, not having this form in place can cause more trouble than you might think.
Let's go over what could go wrong if you don't employ HIPAA release forms.
Legal risks and penalties
Without a signed HIPAA release form when sharing PHI, there may be severe legal consequences. HIPAA violations can result in penalties ranging from hefty fines to criminal charges, depending on the severity and intent of the violation.
Fines can go as high as $1.5 million per year for violations of an identical provision.
Loss of trust
Patient trust is crucial in healthcare. Failure to obtain proper authorization before sharing PHI can lead to a breakdown in the patient-provider relationship. This could take years to rebuild.
Impact on professional reputation
Negative publicity affects the covered entity and the individual professionals responsible for patient data handling. This can have long-term repercussions for the medical brand and individual career opportunities.
Operational delays
Medical procedures or healthcare services requiring PHI sharing may be delayed when a HIPAA release form is absent. Without this information-sharing process in place, it creates room for inaccurate or incomplete information capture.
Ultimately, this affects patient care and adds to operational inefficiencies.
Audit failures
HIPAA mandates regular audits of healthcare entities to ensure compliance. The absence of required HIPAA release forms can lead to audit failures, subjecting the organization to additional scrutiny and potential penalties.
Data integrity and security risks
Unauthorized sharing of PHI compromises patient privacy and poses data integrity risks. Without formal consent, it becomes harder to maintain an accurate record of data disclosures, increasing the risk of data breaches.
Having a signed HIPAA release form for every instance where PHI is shared, you underscore your commitment to compliance and patient-centric care.
When HIPAA release forms aren't required
Even in the complex field of healthcare, there are scenarios where a HIPAA release form isn't needed, particularly in medical app development.
Below, we'll discuss some of those scenarios.
De-identified information
If the information has been de-identified according to HIPAA standards, it's no longer considered PHI and doesn't require a HIPAA release form for sharing.
De-identification involves removing personally identifiable information (PII) such as name and surname, phone number, address, social security details, etc.
According to the HIPAA, there are two main methods for de-identifying PHI:
- Expert determination: Hiring a person with appropriate knowledge and experience in statistical and scientific principles to certify that the data has a minimal risk of being re-identified.
- Safe harbor method: Removing 18 types of identifiers listed by HIPAA, such as names, geographic data smaller than a state, dates directly related to an individual (like birth date), telephone numbers, social security numbers, email addresses, and others.
Emergency situations
The HIPAA allows for disclosing PHI without consent in specific emergencies, as long as the sharing complies with particular conditions in the HIPAA privacy rule.
Such events or circumstances include:
- Immediate threats to health or safety: PHI can be disclosed when there's a pressing and immediate threat to an individual's health or safety, such as life-threatening injuries or acute medical conditions.
- Public health emergencies: In the case of epidemics or pandemics, PHI may be shared to control the spread of disease, often in coordination with public health agencies.
- Natural disasters: In circumstances like hurricanes, earthquakes, or floods, PHI can be disclosed to coordinate patient care and locate missing persons.
- National security: In the interest of national security, PHI can be shared with authorized federal officials.
- Law enforcement: If a person is a suspect, victim, or witness in a criminal activity that has resulted in injury, PHI may be disclosed to law enforcement.
- Organ transplants: In urgent cases of organ, eye, or tissue donation and transplantation, PHI can be disclosed to facilitate the process.
- Firearm injuries: Some states mandate reporting gunshot wounds and similar injuries to law enforcement, which can involve sharing PHI.
- Overdose cases: In the event of drug overdoses, PHI may be disclosed to medical personnel or law enforcement for prompt intervention and harm reduction.
- Mental health crises: In the case of an immediate threat to oneself or others due to a mental health condition, PHI can be shared to mitigate the risk.
- Child abuse or neglect: If healthcare providers believe a child is a victim of abuse or neglect, PHI may be disclosed to protect the child.
- Adult and domestic abuse: Similar to child abuse, cases involving abuse or neglect of vulnerable adults may necessitate sharing PHI without consent.
Within the same healthcare entity
In many cases, PHI can be shared within the same healthcare entity for treatment, payment, or operational purposes without needing a separate HIPAA release form.
User-initiated sharing
In some medical apps, users voluntarily share their information with third parties. In these cases, developers often include explicit statements clarifying that users are choosing to share their data.
This consent bypasses the need for a separate HIPAA release form.
Public health and research
Specific provisions in HIPAA allow PHI to be shared for public health activities and research without requiring a release form, provided that certain criteria are met.
Criteria for public health activities:
- Mandatory reporting (e.g., contagious diseases or workplace injuries)
- Public health emergencies
- Prevention and control
- Government programs
- Oversight
Criteria for health research:
- Institutional Review Board (IRB) or privacy board approval
- Only accessing the minimum data necessary to reach research objectives
- De-identification
- Limited data sets
- Preparatory research
- Research within the same institution
By understanding when a HIPAA release form is and isn't necessary, you can streamline your process and resource allocation, ensuring that you focus on compliance where it’s most needed.
HIPAA technicalities and terminology
The other term often used for a HIPAA release form is "Authorization." This authorization allows covered entities to use or disclose PHI for the particular purposes we've discussed.
Navigating the complexities of HIPAA compliance requires more than a surface-level understanding of the regulations. Let's demystify some of the common technicalities and terminologies you'll encounter.
Protected Health Information (PHI)
We've used this term already, but what exactly is PHI?
This term refers to any information identifying an individual and relating to their past, present, or future physical or mental health condition, including healthcare services and payments.
Business Associate Agreement (BAA)
When a third-party service provider can access PHI, a Business Associate Agreement (BAA) must be signed. This document details the responsibilities and required security measures for both parties.
Minimum necessary rule
This principle dictates that only the minimum necessary information required to complete a task should be disclosed.
Developers need to implement this at code level to limit access permissions.
Data encryption
Ensuring that PHI is encrypted both at rest and during transmission is critical. Encryption algorithms like AES (Advanced Encryption Standard) with 256-bit keys are generally considered secure.
Access control
This term refers to mechanisms like authentication and authorization that limit who can access PHI. Two-factor authentication (2FA) and role-based access are common strategies implemented for this.
Audit trail
An electronic record that chronicles user activity related to PHI. It's essential for tracking unauthorized access and providing documentation during compliance audits.
Risk assessment
A comprehensive evaluation of potential risks and vulnerabilities to PHI within your system. This is often a prerequisite for determining what security measures must be implemented.
De-identification
The process of removing or altering information that identifies an individual, making it impossible to connect the data back to them. De-identified information isn't subject to HIPAA regulations.
Security rule and privacy rule
The HIPAA security rule outlines the administrative, physical, and technical safeguards for PHI. The privacy rule regulates who's authorized to access and control this information.
Covered entities
As mentioned earlier, covered entities are the primary bodies that must be HIPAA-compliant. This includes healthcare providers, health plans, and healthcare clearinghouses.
Consent vs authorization
Though these terms are often used interchangeably, there's a nuanced difference.
Consent generally refers to agreeing to allow something to happen, while authorization is a more formal agreement, often requiring documentation like a HIPAA release form.
Understanding the common terms and technicalities will help you navigate HIPAA compliance and be better prepared to build and manage secure healthcare systems.
Now, we’ll look at what form fields to add to a HIPAA release form to ensure you capture the necessary medical information.
What information must be included in a HIPAA release form?
If you're building your own authorization form from scratch or customizing a template, we recommend the following form fields and security measures.
Essential form fields for HIPAA compliance
Your HIPAA release form must be detailed, outlining the specifics of the information to be shared. Here are the fundamental components to include:
- Patient's name and identification: A clear identification of the individual whose information will be shared.
- Recipient information: Information on the covered entity that will be authorized to receive the PHI.
- Type of information: A detailed account of what kind of information will be shared, such as medical records, laboratory results, etc.
- Purpose: The reason or specific use for the PHI disclosure.
- Expiration date: An expiry date or an expiration event related to the individual or the purpose of the use or disclosure.
- Signature: The patient’s dated signature or that of the patient’s representative if the patient is unable to sign. This may be a hand-written signature or a digital signature.

HIPAA release form checklist for developers
Developers and product managers must put measures in place to control how data is captured, encrypted, and transmitted, ensuring the patient authorization form is easily accessible and user-friendly.
- Validation rules: Implement validation rules to ensure all mandatory fields are filled out.
- Encryption: Secure the data both at rest and in transit.
- Accessibility: Ensure the form is accessible to all users, including those with disabilities. Accessibility features like screen reader compatibility are not just nice-to-haves; they're mandated by law in many jurisdictions.
- User authentication: Use multi-factor authentication (MFA) to confirm the identity of users with access to the data.
- Data backup: Regularly back up data and ensure the backups are also HIPAA-compliant.
- Revocation option: Include an easily accessible option for patients to revoke their authorization, as mandated by HIPAA.
- Transparency: Offer a clear and understandable privacy policy, which should be easily accessible through the form interface.
- Localization: If your application will be used in different jurisdictions, make sure that the form complies with local laws and regulations in addition to HIPAA.
- Data breach protocols: Have a well-defined procedure for identifying and responding to potential data breaches.
How to integrate HIPAA release forms into your systems
What's your particular application for your HIPAA release form? Perhaps it's part of consent to digital marketing communication from a covered entity or separate consent for treatment requiring the patient's signature.
The communication delivery depends on your tech stack and how the data needs to be used.
You can take an integrated approach to HIPAA compliance and rely on a third-party form-building tool like Feathery.
With Feathery, you can create bespoke branded HIPAA release forms to garner medical information and patient consent securely. Our forms can be embedded on your website or app and integrated with other tools in your stack.
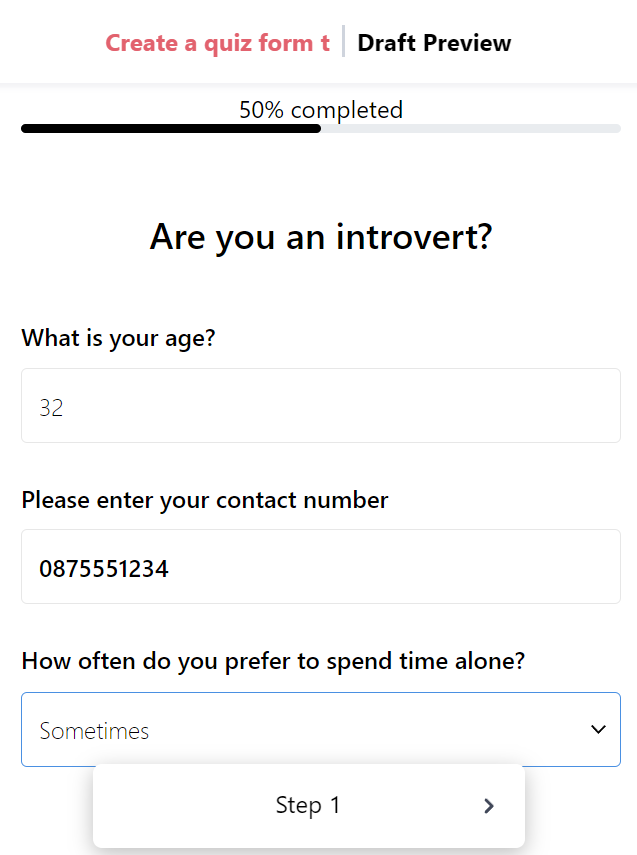
See how Feathery works in the interactive demo below:
Rely on APIs and embedded forms
Consider using APIs and middleware solutions that are HIPAA-compliant. These can be the glue between your EHR systems and the release form, ensuring smooth data transfer.
Set up a seamless workflow
Develop a workflow that prompts users to complete the HIPAA release form at the appropriate stage of interacting with your platform. It should be integrated seamlessly so as not to disrupt the user experience.
Implement audit trails
As part of your system, include a comprehensive audit trail that tracks who accessed what information, when, and why. This will maintain your system's integrity and make it easier to provide proof if disputes arise.
Best practices for developing HIPAA-compliant release forms
Now that you have enough information and tools to create and implement HIPAA release forms, we'd like to share some practical tips.
Following these best practices will help you design forms that are not only compliant but also user-friendly.
1. Design with the user in mind
For an effective HIPAA release form, usability should be your guiding principle. The design must be intuitive, and users should be able to complete the form without a tutorial.
You can show or hide form fields based on user input so they only see the relevant fields to fill out.
The amount of information needed can be overwhelming. We highly recommend breaking your HIPAA release form down into multiple steps with only 1–5 questions visible at any time. This creates the impression that the form isn't very long and lets the user focus on the questions immediately in front of them.
You can add a progress bar at the top of your multi-step release form to guide the user through the process.
2. Robust security measures
Implementing strong security protocols is non-negotiable. Utilize encryption algorithms that are in line with industry standards. Also, we suggest keeping a log of all activities on the form – this will help you troubleshoot any issues or security breaches.
3. Testing
Before going live, the form should undergo rigorous testing to identify potential security loopholes, validate functionality, and ensure its ease of use.
With Feathery, you have the option to preview your form in a live test environment before publishing it. You can also toggle desktop and mobile view in the Designer to ensure all fields are accessible and functional on different screen sizes.
4. Keep your release form up to date
HIPAA regulations are not static; they evolve. Continually update your authorization forms to comply with any new amendments to the HIPAA.
If your form is used in other jurisdictions, you should also regularly check and ensure it's fully compliant with applicable laws.
Common mistakes to avoid when developing a HIPAA release form
Lack of transparency
One of the frequent mistakes healthcare organizations make is not being transparent with patients about how their information is used.
To nurture a trusting relationship with all your clients or patients, always provide a clear and easy-to-understand explanation on the form itself.
Inadequate security protocols
Neglecting to implement robust security measures is a one-way ticket to compliance failure and legal troubles. This includes weak encryption methods and insufficient access controls.
Overlooking version control
When updates to the HIPAA regulations occur, your forms need to reflect those changes. Failure to manage versions can result in using outdated forms that aren't compliant.
Ignoring mobile responsiveness
With increasing numbers of users accessing healthcare platforms via mobile, mobile responsive design is becoming increasingly vital. Your HIPAA release form should be easily accessible and functional on all devices.
Your next step to HIPAA compliance
In the healthcare industry, trust is the most valuable commodity you have. Developers and product managers in the healthcare sector are responsible for safeguarding some of people's most sensitive information.
Navigating the intricacies of HIPAA compliance can be daunting, but it doesn't have to be. Understanding what a HIPAA release form is, why it's essential, and how to properly develop and integrate one into your system makes a notable difference in your design and delivery.
By adhering to best practices and avoiding common mistakes, you can build a robust, compliant, and user-friendly platform that upholds patient data integrity.
Feathery's secure and compliant form builder empowers you to create HIPAA release forms using an easy drag-and-drop interface. We also offer many other customizable form templates and sophisticated CSS styling tools.
Are you ready to try Feathery for medical data-sharing authorization? Create a free, secure form.




.svg)

